Oral cancer is a serious condition affecting the mouth and throat region, and expert care by Dr Tulika Dubey offers a pathway to early diagnosis and effective treatment. This guide covers every aspect of oral cancer: what it is, risk factors, signs and symptoms, diagnostic steps, staging, treatment options, survival outlook, prevention strategies and how Dr Tulika Dubey’s approach brings value to patients.
Introduction
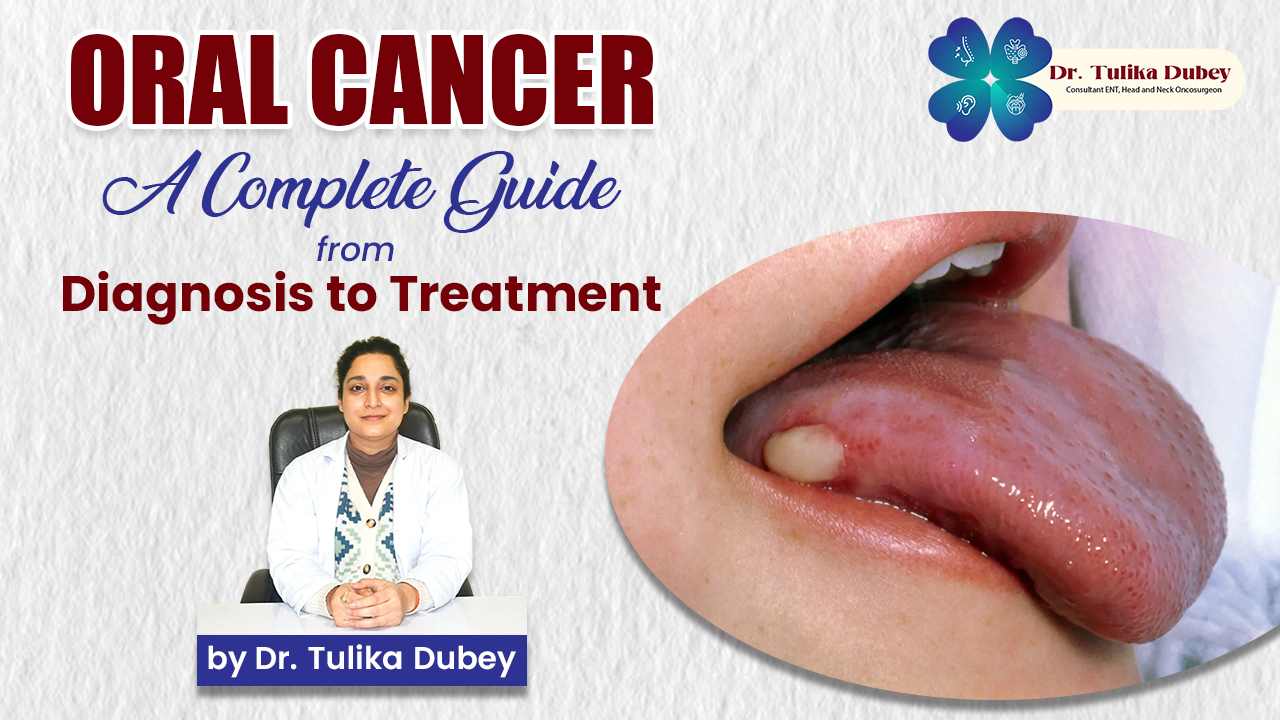
Oral cancer refers to malignant growths in the oral cavity including the lips, tongue, gums, floor of mouth and inner cheeks. With early detection, oral cancer is among the more treatable cancers of the head and neck region.
Dr Tulika Dubey brings expertise in head and neck onco-surgery and oral cavity tumours, guiding patients through multidisciplinary care, tailored prevention and treatment plans.
What is Oral Cancer?
Oral cancer includes cancers that originate in cells of the mouth or throat. Most commonly, they are squamous cell carcinomas, arising in the thin, flat cells that line the lips and mouth interior.
Locations of oral cancer may include:
- Lips
- Tongue (especially the undersurface and sides)
- Floor of the mouth
- Inner lining of the cheeks (buccal mucosa)
- Gums (gingiva)
- Roof of the mouth (hard palate)
- The back of the mouth (oropharynx)
The pathophysiology involves abnormal changes in the DNA of oral epithelial cells, causing growth of malignant tissue, tumour formation and the potential for spread (metastasis).
Risk Factors for Oral Cancer
Identifying risk factors is critical for prevention and early detection. Dr Tulika Dubey emphasises a comprehensive review of risk factors to stratify patient risk and advise on lifestyle modification. Key risk factors include:
Tobacco Use
The use of tobacco (smoking cigarettes, cigars, pipes, chewing tobacco, snuff) is the single greatest risk factor for oral cancer.
The synergy between smoking and another risk (such as alcohol) increases risk significantly.
Alcohol Consumption
Frequent and heavy alcohol intake increases the risk of mouth cancer. The combined use of alcohol and tobacco multiplies the risk.
Human Papillomavirus (HPV) Infection
Infection with HPV especially HPV‑16 is increasingly recognised as a risk for certain oral and oropharyngeal cancers.
Sun (Ultraviolet) Exposure
Lip cancer risk is elevated by prolonged UV light exposure on the lips, especially in fair‑skinned individuals.
Immune Suppression and Other Factors
Conditions such as immune‑weakening diseases, nutrition deficiencies, poor oral hygiene, chronic irritation of the oral mucosa also contribute.
Regional/Habit‑Specific Risks
In some regions, habits such as betel quid chewing or areca nut use significantly increase oral cancer risk (especially in South and Southeast Asia). Incorporating local risk profiling is part of Dr Dubey’s practice.
Signs and Symptoms of Oral Cancer
Recognising the early warning signs is critical because early‑stage oral cancer has a much better prognosis. Dr Tulika Dubey emphasises vigilant screening and patient education for early detection. Common signs include:
- A sore or ulcer in the mouth that does not heal within two weeks.
- White or red patches (leukoplakia or erythroplakia) on the oral mucosa or tongue.
- A growth or lump inside the mouth.
- Loose teeth or changes in how dentures fit.
- Difficulty or pain when swallowing, speaking or moving the jaw/mouth.
- Ear pain (referred), unexplained weight loss or persistent sore throat.
- Swelling, lumps in the neck (lymph nodes) due to spread of disease.
Because many common benign conditions also affect the mouth, Dr Dubey stresses that persistent signs (lasting more than two weeks) must trigger specialist evaluation.
Diagnosis and Staging of Oral Cancer
When signs raise concern, a systematic approach to diagnosis and staging ensures optimal treatment planning. Dr Dubey’s clinic offers structured diagnostic pathways:
Clinical Examination
Detailed inspection of the oral cavity, lips, tongue, cheeks, floor and roof of mouth, gums and neck lymph nodes. The examination may also include evaluation of dental and prosthetic status, and review of risk history.
Biopsy and Histopathological Evaluation
Tissue sampling (biopsy) is essential to confirm malignant cells, determine histologic type (most often squamous cell carcinoma) and grade the tumour.
Imaging and Tests
To determine the tumour extent (size, invasion) and spread, imaging may include CT scan, MRI, PET scan and ultrasound of neck nodes.
Staging considers tumour size, lymph node involvement and presence of distant metastasis. Early‑stage (Stage I/II) disease has better outcomes; advanced stage (Stage III/IV) requires more complex treatment.
Role of Oral Cancer Specialist
Dr Tulika Dubey works with a multidisciplinary team of surgeons, radiation oncologists, medical oncologists, dental specialists and speech/rehabilitation therapists to interpret staging and plan management.
Treatment Options for Oral Cancer
Treatment of oral cancer is tailored according to the stage, location, patient health status and functional considerations such as speech and swallowing. Dr Tulika Dubey ensures treatment is evidence‑based and aligned with patient goals. Key treatment modalities include:
Surgery
Surgery is often the first‑line approach for accessible tumours of the oral cavity. Removal of the primary tumour and sometimes neck lymph nodes (if involvement) is standard.
Reconstructive surgery (e.g., grafts, flaps) may be needed to restore appearance and function after tumour removal in the mouth.
Radiation Therapy
Radiation therapy may be used alone for small tumours or as an adjunct post‑surgery to reduce recurrence risk. Functional preservation (of speech, swallowing) is a key consideration.
Chemotherapy
For advanced disease, or when tumours have spread to neck nodes or distant organs, chemotherapy (sometimes in combination with radiation) becomes part of the treatment plan.
Combined Modality Treatment
Many cases require a combination of surgery + radiation ± chemotherapy. Dr Dubey coordinates multi‑modal care to optimise outcome while minimizing complications.
Emerging & Supportive Treatments
- Targeted therapy and immunotherapy are evolving in oral cancer management (especially for recurrent or metastatic disease).
- Speech, swallow rehabilitation, nutritional support, dental rehabilitation and psychosocial care are integral to holistic recovery.
Survival Rates and Prognosis
The prognosis of oral cancer depends heavily on early detection and stage at diagnosis. Data suggest that when confined to the primary site (early stage), the survival rate is higher.
Dr Tulika Dubey emphasises that with expert care, early‐stage diagnosis can lead to excellent outcomes in terms of survival, function and quality of life.
Advanced disease (spread to lymph nodes or distant sites) reduces survival rates and complicates functional outcomes; therefore prevention, screening and early referral are critical.
Prevention and Early Detection

Prevention and screening serve as linchpins in reducing the burden of oral cancer. Dr Tulika Dubey’s preventive strategy encompasses patient education, risk reduction and routine oral examination. Components include:
- Cease tobacco use (smoking or smokeless) this remains the most impactful prevention step.
- Moderate or eliminate alcohol consumption.
- Maintain good oral hygiene and regular dental check‑ups; dentists or specialists can perform oral cancer examinations during routine visits.
- Protect lips from UV exposure (e.g., broad‑brimmed hat, lip sunscreen).
- Vaccinate for HPV where indicated (reducing HPV‑related oral cancers).
- Educate about early signs of oral cancer and encourage prompt specialist referral for persistent lesions.
Why Choose Dr Tulika Dubey for Oral Cancer Care

Expertise in oral cancer management demands not only technical skills but multidisciplinary coordination, patient‑centred care and holistic support. Dr Tulika Dubey stands out in several ways:
- Specialized training and experience in head‑and‑neck onco-surgery, with focus on oral cavity tumours.
- Collaborative treatment planning: coordinating surgery, radiation, medical onco-surgery, dental rehabilitation and functional recovery.
- Emphasis on voice, swallowing and quality of life outcomes in addition to survival.
- Preventive focus: embedding risk‑factor assessment, screening and patient education in clinical workflow.
- Personalized care: tailoring treatment to tumour characteristics, patient comorbidities, functional goals and preferences.
Patients managed under Dr Dubey’s care receive comprehensive pre‑treatment counselling, detailed explanation of treatment options, side‑effects and long‑term follow‑up plans.
Post Treatment Follow‑Up and Survivorship
Oral cancer care does not end when treatment ends. Dr Tulika Dubey’s practice emphasises robust follow‑up in order to monitor for recurrence, manage late‑effects and support return to normal function.
Key elements include:
- Regular physical exams of the mouth, throat and neck.
- Imaging or other investigations as indicated to detect recurrence early.
- Rehabilitation services: speech therapy, swallow therapy, dental prosthetics and restorative work.
- Nutritional counselling, psychosocial support and lifestyle modification (tobacco/alcohol cessation).
- Monitoring for second primary cancers (oral cancer patients are at higher risk).
- Long‑term monitoring of functional outcomes: chewing, speech, aesthetics, social reintegration.
Challenges in Oral Cancer Management
Despite advances, oral cancer presents challenges which Dr Tulika Dubey addresses proactively:
- Late presentation: Many cases present at an advanced stage due to low awareness of early signs.
- Functional impact: Tumours in the mouth affect speech, swallowing, eating, aesthetics requiring complex rehabilitation.
- Recurrence and secondary tumours: Need for vigilant monitoring.
- Cost and resource intensive treatment: Reconstruction, multidisciplinary care and long‑term support require coordination.
- Psychosocial aspects: Quality of life, body image, return to nutrition and speech are major concerns.
Dr Dubey’s approach incorporates prehabilitation (pre‑treatment counselling and therapy), advanced reconstructive techniques, and integrated rehabilitation pathways.
Emerging Trends and Research
Research in oral cancer is advancing rapidly, opening new dimensions that Dr Tulika Dubey monitors and integrates into practice:
- Enhanced imaging and diagnostic tools aim to detect oral cancer earlier and more accurately.
- Artificial intelligence (AI) and machine learning models are being developed to predict oral cancer outcomes and assist screening.
- Research into the role of HPV vaccines in reducing oral cancer incidence is ongoing.
- Precision oncology: treatment tailored to genetic and molecular characteristics of the tumour promises better outcomes.
- Functional rehabilitation technologies continue to evolve: speech/swallowing robotics, 3D‑printed oral prosthetics, virtual therapy.
Oral Cancer in the Nepalese Context
In Nepal and surrounding regions, the incidence of oral cancer remains significantly high due to widespread use of smokeless tobacco, betel quid (paan), and areca nut. These culturally entrenched habits contribute to elevated oral cancer risk, particularly in rural and semi-urban areas.
Dr Tulika Dubey’s practice integrates region specific awareness and prevention strategies, focusing on the unique lifestyle and risk factors prevalent in Nepal. Screening and education programs are culturally adapted to address these habits, empowering early detection and lifestyle modification within high risk communities.
Practical Checklist for Oral Cancer Awareness
Below is a summary checklist extracted from Dr Tulika Dubey’s patient education resources to empower early detection and prevention:
- Quit tobacco in all forms (smoked, sniffed, chewable).
- Limit alcohol consumption; avoid heavy, frequent use.
- Maintain regular dental check ups and request an oral cancer screening.
- Be alert to any mouth sore, white/red patch, lump or change in dental fit which persists beyond two weeks.
- Protect lips from sun exposure (use lip sunscreen, wear hats).
- Ask about HPV vaccination if age and risk permit.
- Follow up promptly with a specialist if any suspicious lesion is found.
- After treatment, commit to regular follow‑up, rehabilitation and risk‑reduction.
Summary
Oral cancer is a serious but treatable disease when detected early. Expert management by Dr Tulika Dubey offers patients comprehensive care from prevention and screening through to diagnosis, treatment, rehabilitation and survivorship. Emphasis on early detection, multidisciplinary coordination, functional outcomes and patient‑centred care make a significant difference in outcomes.
Lifelong vigilance, regular screenings, risk factor reduction and specialist care represent the best strategy to tackle oral cancer effectively.